If you and your partner have been trying for a baby for a while and it’s not happening, it can feel brutally unfair. Especially when you’re doing all the “right” stuff and still getting nowhere. One of the most common surprises for couples is that male factors are often part of the story, and sometimes they’re fixable.
This is a sensitive topic, so I’m going to keep it practical and straight: what low sperm count or quality actually means, what can cause it, and what tends to help.
What “Low Sperm Count Or Quality” Actually Means
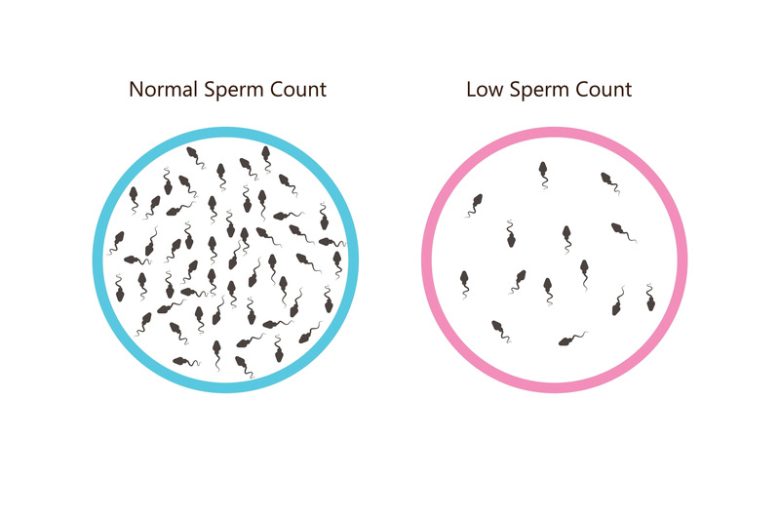
When people say “low sperm count”, they usually mean one or more results on a semen analysis are below the lower reference limits. A semen analysis looks at things like:
- Sperm concentration: how many sperm per millilitre
- Total sperm number: how many sperm in the whole sample
- Motility: how well they move (especially progressive motility, meaning they swim forward)
- Morphology: the percentage that look “normal” in shape
Current World Health Organization (WHO) 2021 lower reference limits often quoted in UK lab guidance include concentration 16 million/mL and total sperm number 39 million per ejaculate (with other parameters assessed too).
You’ll also see terms like:
- Oligozoospermia: low sperm count
- Asthenozoospermia: poor motility
- Teratozoospermia: poor morphology
- Azoospermia: no sperm seen in the ejaculate (rare, but important to assess properly)
One key thing: a “below range” result doesn’t automatically mean “can’t have kids”. It means the odds may be lower, and it’s worth investigating and improving what you can.
Why It Happens

There isn’t one single cause. It’s usually a mix of biology, health, lifestyle, and sometimes plain bad luck.
Heat And Testicular Temperature
Sperm production is temperature-sensitive. The testes sit outside the body for a reason: they work best a bit cooler than core temperature. Regular exposure to heat (hot tubs, saunas, very hot baths, some work environments, tight clothing in some cases) can affect semen parameters, and there’s evidence this can be reversible for some men once the heat exposure stops.
Varicocele
A varicocele is basically enlarged veins in the scrotum (a bit like varicose veins). It’s common, and in some men it’s linked with poorer sperm parameters, possibly because it interferes with temperature regulation and increases oxidative stress.
Not every varicocele needs treating, and different guidelines emphasise different approaches, but it’s one of the classic “don’t miss this” things in a male fertility work-up.
Smoking, Vaping, Alcohol, And Drugs
Smoking is consistently linked with poorer semen quality, and stopping is a straightforward win if you’re trying.
Alcohol is trickier because “small amounts” aren’t the same as “heavy drinking”, but UK NHS advice for men with low sperm count includes drinking less and keeping within 14 units a week, spread out.
Cannabis has mixed evidence overall, but enough studies suggest a potential negative impact on semen parameters that most fertility clinics will advise cutting it out while trying.
Weight, Diet, And Metabolic Health
Higher BMI is associated with worse semen parameters in many studies, likely through hormone changes and inflammation. Even modest weight loss can help overall reproductive health.
Diet matters too, mostly because sperm are vulnerable to oxidative stress and inflammation. NHS fertility leaflets generally push the same foundations you’d expect: balanced diet, fewer ultra-processed foods, and practical lifestyle changes.
Hormones, Infections, And Medical Conditions
Low testosterone or other hormone issues can reduce sperm production. Infections and inflammation can also play a role (sometimes without obvious symptoms). And then there are structural problems (blockages), genetics, undescended testes history, or past chemo/radiotherapy. These are the reasons it’s worth getting properly assessed rather than assuming it’s “just lifestyle”.
One massive, easily-missed one: testosterone therapy and anabolic steroids. External testosterone can shut down sperm production by suppressing the signals the testes need to make sperm. If you’re on testosterone or have been using anabolic steroids, tell your doctor early, because it changes the plan.
The Bit That Gives You Hope: Sperm Can Improve

Sperm production runs on a lag. From the start of development to mature sperm is commonly cited as around 74 days, so changes you make now often show up around the 2–3 month mark.
So if you’re going to go all-in on improving things, think in “the next 12 weeks”, not “the next 12 days”.
What You Can Do To Improve Sperm Count And Quality
Stop Smoking And Cut Down Alcohol
If you do one thing: stop smoking. If you do two things: stop smoking and get alcohol under control. The NHS advice for low sperm count specifically calls these out.
Get Your Weight And Fitness Into A Sensible Place
You don’t need to turn into a monk or a marathon runner. The point is to improve metabolic health: consistent movement, a healthy weight range for you, and avoiding extremes (crash dieting and overtraining can backfire). NHS fertility guidance often frames this as getting as close to a healthy BMI as you realistically can.
Protect Your Testes From Heat
If you’re doing regular hot tubs/saunas or very hot baths, pause it while trying. If your job involves heat exposure, talk through mitigation (breaks, cooling, protective measures). This is one of the few “small change, potentially decent upside” moves.
Check Meds And Supplements With A GP
Some prescribed medications can affect ejaculation, hormones, or semen parameters. Don’t stop anything abruptly, but do a proper medication review.
Be cautious with supplements. The Cochrane evidence on antioxidants suggests they may improve outcomes like pregnancy or live birth in subfertile men, but the certainty of the evidence is very low, and studies vary a lot. In other words: not snake oil, but not a magic fix either.
If you do try a supplement, treat it as an add-on to lifestyle changes, and ideally run it past a clinician (especially if you have medical conditions or take regular meds).
Get Properly Assessed
If you’ve been trying for 12 months with regular unprotected sex (or 6 months if your partner is 35 or older), most major health bodies recommend evaluation.
And if a semen analysis is abnormal, that’s not the end of the road. It’s the start of figuring out why. That can include repeat testing (because samples vary), examination for varicocele, hormone blood tests, and sometimes genetic or imaging tests if counts are very low.
If You Take One Thing Away
Low sperm count or poor sperm quality is common, it’s often multifactorial, and it can improve. Focus on the boring fundamentals for 12 weeks (no smoking, sensible alcohol, healthier weight, avoid heat, better sleep and diet), and in parallel push for a proper medical assessment so you’re not missing something treatable like a varicocele, hormone issue, infection, or medication effect.
If you want, paste the exact semen analysis parameters you were given (you can remove any personal identifiers) and I’ll explain what each number usually means and what questions it should prompt at a GP or fertility appointment.